Abstract

Introduction
Primary central nervous system lymphoma (PCNSL) is a rare extra-nodal non-Hodgkin lymphoma involving the brain, leptomeninges, eyes or spinal cord without evidence of primary site out of CNS. This disease is thought to have a distinct biological behavior and shows unsatisfactory outcomes comparing to other types of non-Hodgkin lymphoma. Several prognostic models have been proposed to predict disease course and survival. In this study, we validated previously studied prognostic models in a single center cohort, and we propose a new prognostic model for PCNSL.
Methods
The registry data set of PCNSL, collected from March 1993 to May 2017 at a single institute, Asan Medical Center, was retrospectively reviewed. Overall survival (OS) was defined as the time from the beginning of first-line therapy to any cause of death, and progression free survival (PFS) was defined as the time from the beginning of first-line therapy to disease progression or death. Univariate and multivariate analyses were performed to identify prognostic factors for PFS and OS using a Cox proportional hazards model. OS and PFS curves were estimated by the Kaplan-Meier method and compared using log-rank tests. All statistical analyses were performed using IBM SPSS version 21.0.
Results
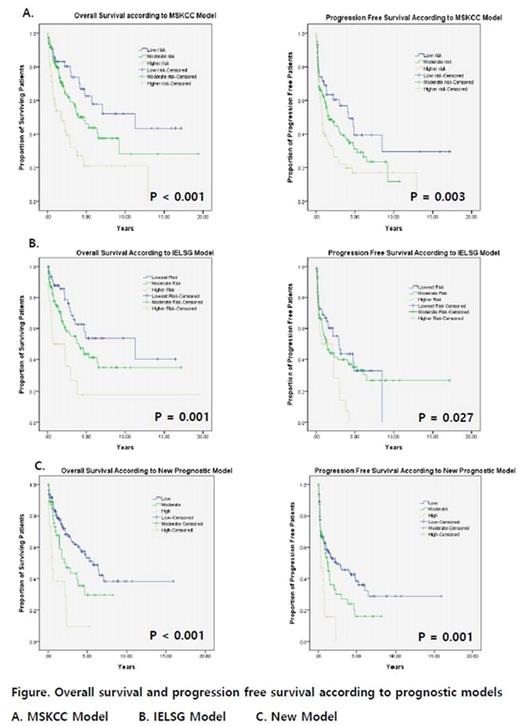
Total 241 patients were identified and enrolled in analyses. Median follow-up duration was 4.3 years (IQR 0.03-19.4), median OS was 3.8 years (95% CI 2.6-5.0), and median PFS was 1.6 years (95% CI 0.8-2.2). Median age was 60 years-old (range, 17-86) and 31.5% of the patients were 65 years or older. One-hundred thirty four patients (55.6%) were male and 88.4% of the patients had confirmed histologic diagnosis of DLBCL type. Seventy patients (29.0%) had ECOG performance status of 2 or worse at the time of diagnosis and 45.6% had multifocal lesions. Most of the patients (94.6%) had chemotherapy as first-line treatment, 71.8% showed overall response (CR or PR) to first-line therapy, and 34.9% of patients had autologous stem cell transplantation. In univariate analyses of prognostic factors, only old age (≥60), poor performance (ECOG PS ≥2), and elevated serum β2 microglobulin (≥1.8 μg/mL) showed statistically significant poor outcome in both OS and PFS with p value of 0.05 or less. In multivariate analyses, poor performance showed significant poor prognosis with HR 2.5 [95% CI 1.6-3.9, p <0.001] and 1.8 [95% CI 1.2-2.6, p = 0.003] in OS and PFS, respectively. Old age showed HR 1.2 [95% CI 0.8-2.0, p = 0.353] and 1.3 [95% CI 0.90-2.0 p = 0.171] in OS and PFS. Elevated serum β2 microglobulin showed HR 1.6 [95% CI 1.0-2.6, p = 0.05] and 1.4 [95% CI 0.9-2.1, p = 0.1] in OS and PFS. We designed new prognostic model consisting of old age, poor performance and elevated β2 microglobulin and presence of each factors meaning for 1 point. Total score from 0-1 was defined as low risk, 2 as moderate risk, and 3 as high risk. Median OS was 5.7 years [95% CI 4.1-7.3], 2.3 years [95% CI 0.9-3.7], and 0.5 years [95% CI 0.2-0.8] for low, moderate, and high risk group comparing between risk groups according to our new prognostic model. Median PFS was 2.3 years [95% CI 0.4-4.3], 1.3 years [95% CI 0.8-1.8] for moderate risk group, 0.4 years [95% CI 0.5-0.7] for low (136 patients), moderate (56 patients), and high risk group (16 patients). Comparison of Kaplan-Meier survival curves with other prognostic models are in following figure.
Conclusion
Old age (≥60 years old), poor performance (ECOG PS ≥2), and elevated β2 microglobulin level (≥1.8 μg/mL) were statistically significant poor prognostic factors of PCNSL. Our new prognostic model could be a good predictive tool of prognosis in PCNSL.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal